Skip NavigationSkip to Primary Content

NVA and Ethos Veterinary Health
A leading global veterinary organization, NVA is excited to announce it will form two distinct businesses, Ethos Veterinary Health (“Ethos”), which will consist of 145 world-class specialty veterinary hospitals, and NVA, which will continue to oversee approximately 1,400 premier general practice veterinary hospitals in addition to equine hospitals and pet resorts. Sharing a love of animals and the people who love them, NVA and Ethos are committed to deliver exceptional care to more patients and elevate the veterinary profession like we have done for more than 25 years. Learn more.
Our mission
To improve the comfort and well-being of pets by providing progressive and compassionate care. We develop a team of individual hospitals and pet resorts that share knowledge to achieve sustainable growth.

Get to Know Us
Founded by a veterinarian for veterinarians, NVA has a rich 25-year history of building a veterinary and pet care community of general practice, emergency, equine, specialty and pet resorts.

Partner With Us
No one understands your unique practice or culture the way you do – but you don’t have to do it alone. By partnering with NVA, we can help you successfully navigate the business side of veterinary medicine.

Work With Us
Turn your love of animals into the career of a lifetime. Join a community of like-minded professionals dedicated to collaboration, innovation, and professional development.
Our people make a real difference in their neighborhoods every day
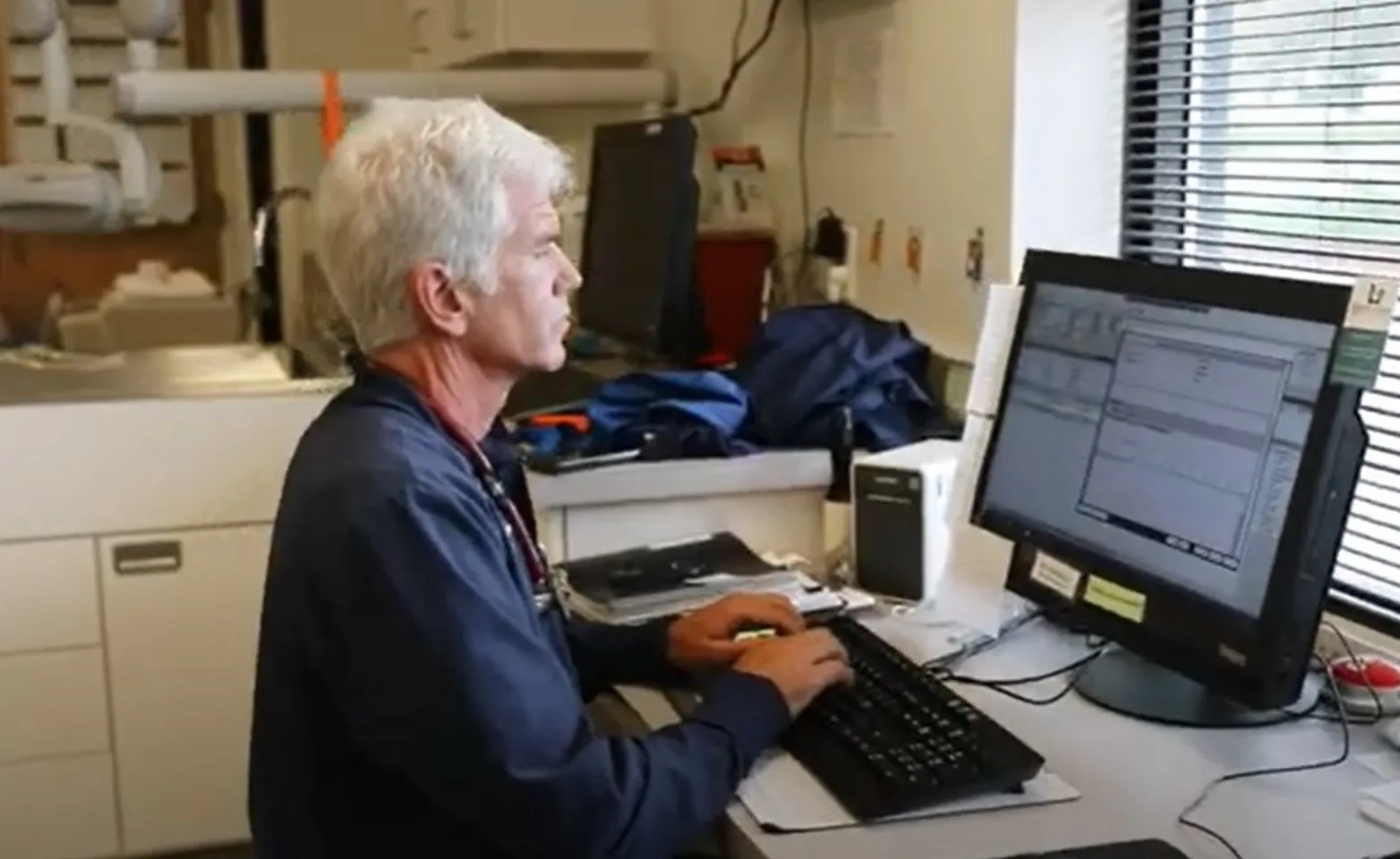
Shoreline Central Animal Hospital
Shoreline, WA
After selling his practice to NVA in 2012, Dr. John Paulson was committed to his life's passion and continuing to work in the profession he loves. Through a new joint-venture partnership with NVA, Dr. Paulson found a renewed purpose and continued success with a trusted partner.

St. Francis Of Assisi Veterinary Medical Center
San Antonio, TX
Dr. Daniel Holub and Dr. Robert Bauml wanted to cash in on their sweat equity with a partner that respected the way they practiced medicine. With NVA, the clinic’s business has almost doubled.

Waterville Veterinary Clinic
Waterville, NY
Looking ahead to retirement, Dr. Dan Gilchrist wanted a partner that would honor his business culture and staff seniority, and allow his son, James, to take over the practice.

North Paw Animal Hospital
Durham, NC
Dr. Gretchen Hutt’s passions include the practice she founded, spending time with her family and traveling the world. Her NVA partnership gives her more time off while maintaining a stable, growing practice.